Acne Scar Treatments At A Glance
- Best Results1-5+ sessions
- Treatment Recovery0-7 days
- Procedure Time30 to 60 min
- Skin SpecialistDermal Therapist, Nurse, Dermatologist
- Duration of ResultsMany years to permanent
- AnaestheticTopical, gas or light sedation
- Back to WorkNext Day- 7 days
- Cost$ - $$$
Acne scars Aims of Treatments
The severity of acne scars should, ideally be an objective measurement, acknowledging subjective perception plays an important role in seeking treatment. If both objective & subjective measurements are similar, successful outcomes can be expected. Various end points have been identified in the scientific literature, as per this landing page.
FactsFacts on scar assessments & end points
- Acne scar severity is both subjectively & objectively measured
- The best results are when subjective & objective viewpoints are aligned
- If you feel that your scars are much worse than what your friends or family members can see, it may show subjective bias of how you perceive scarring
- Having realistic end points & goals are paramount to achieving an exemplary outcome
- It is important to choose a specialist that you entrust & feel comfortable with
How do I measure the severity of acne scars?
There are many ways to gauge severity of scars, including classification. Understandably Medicare is super strict on the measurement of scars as in Australia there is currently a subsidy for the management of objectively severe acne scars. This is where it gets tricky as some good peer reviewed articles (International publications), differ from the opinion of Medicare auditors. For example Grade 1 scars are considered as pigment changes, & as such patients with pigment (either PIH-brown pigment or PIE red pigment) are not entitled to a rebate because contour changes are NOT significant enough to warrant a higher (& more severe) classification. Despite good publications reflecting the quality of life index in patients with pigmented scars, Medicare views these as insignificant to cause true impairment & hence no rebate applies.
On the basis of Medicare requirements, I largely agree with the Goodman-Baron classification in the context of contour changes. In fact I think the classification of Grade 4 scarring is too generous (non-distensible scars not coverable by makeup or the growth of beard hair in men at a distance of 50 cm / conversational distances). Personally I feel that conversational distance is > 75 cm. Regardless, this is the grading I use.
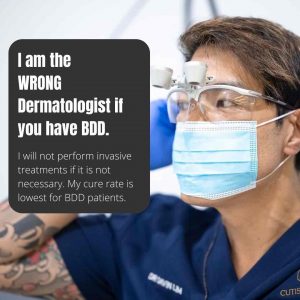
There are other ways to assess the severity of scars, apart from objective photographic documentation. Impact on the QOL or Quality of Life is another way of gauging scar severity as are subjective measurements or perception of scarring. I am not in favor of the later as there may be an overlap with BDD or body dysmorphic disorder. Now, if QOL matches with the Goodman Baron score, I will be able to assist. If QOL does not match up with the objective way of measuring acne scar severity, I may not be the specialist for you. This does not mean you can not have your scars treated, it just means that the methods I employ may not be the optimal way to approach your type of scarring. A good guide as to the actual severity of your scarring may involve asking a close friend, family member or partner to assist.
There are other academic methods to assess the success or failure of scar direct treatment modalities, including lesion count. Though accurate if executed correctly, this is not a practical method to assess end points, as some patients may have >300 scars.
In summary, an objective measurement is both practical & realistic, as the goal of scar revision is to give patients the confidence and knowledge that scars may not be perceivable by others at conversational distance. Scar revision, in the method of which I practice, is not designed to pick up scarring at the worst possible lighting at distances that break the conversal barrier. Once again, there is nothing wrong with this assessment (as it is subjective), however as a specialist dermatologist, this is not the end point of which I practice my trade. Of note, there may be other specialists who may take your case on, alternatively I may refer you to my nursing team for fractional lasers, RFM, RF, microneedling & other modalities.
Bottom line? A therapeutic relationship must be established to meet the same end goals & expectations. I will not subject patients with objectively mild scars to surgical procedures or highly aggressive resurfacing.
What if I perceive my scars are more severe than what my family-friends perceive?
One of two things, firstly you may have over supportive & super nice relationships – this is understandable, secondly you may have an element of Body Dysmorphic Disorder or BDD. This condition is more common than you think, & can manifest itself with preoccupation with acne scarring & or pore sizing (pore phobia) that is subjectively much worse than objective measurements. Some of the signs & symptoms of BDD include-
Preoccupation with appearance: People with BDD are preoccupied with one or more aspects of their physical appearance, believing that these areas look abnormal, deformed, or extremely disfigured (as with acne scarring). People with BDD obsess about the disliked areas, commonly for at least an hour a day (and typically much more).
Insight Regarding BDD Beliefs: Most people with BDD are mostly convinced or completely convinced that they look abnormal or extremely scarred, even though other people don’t see them this way.
Repetitive Compulsive Behaviors: BDD preoccupations fuel repetitive compulsive behaviors that are intended to address, hide, inspect, or obtain reassurance about the disliked body parts. On average, these behaviors take part several times a day. They are usually difficult to control or stop. These behaviors may include the following:
- Social anxiety & distancing (This is different from real pathology where patients with significant scarring & loss of confidence are socially isolated from the mental impact of objectively severe scars).
- Seeking multiple procedures from specialists or experts in the field (This is different from real pathology where treatments in the past are ineffective in the fight against objectively severe acne scars).
- Preoccupied with methods to cover scars, once again different from employing camouflage to hide objectively severe acne scars.

BDD patients often have poor insight into their condition, ofen refusing the help from family, friends & professionals. I am not a BDD expert, however, I may have more experience in the assessment of acne scars than most physicians.
If you do suffer from BDD, I may elect not to treat you, based upon ethical grounds & my mode of practice. This does NOT mean I will not help you, it simply means I will not employ invasive techniques to treat your type of scarring. I will also offer you psychological & psychiatric help, as management of BDD is beyond my scope of expertise. If you have objectively mild scarring, I will not subject you to unnecessary expenses nor invasive surgical techniques to treat your scarring. Instead I may point you towards ‘lighter’ & more cost effective methods such as fractional lasers.
How can I treat mild to moderate scars?
Fortunately, most cases of acne scarring are superficial & do not require surgical key hole subcision. Simple at home microneedling (0.25 mm Dermaroller from eBay cost $5 to 7 dollars) can improve mild textural changes. Please refer to my videos on safe DIY microneedling.
If you have mild to moderate superficial scars, my clinical nurses can assist you. These nurses have been trained in my methodology of scar revision for the past 6 years. We all employ the same manual methods of TCA application, as well as devices such as Genius RF, Infini RF, Fraxel laser (overrated), CO2 CORE, CO2 Mixto, Erbium Sciton Joule, eCO2, Ultrapulse CO2, Pico lasers, eMatrix, Dermapen, Skinpen, LLEDs, Healite, Kleresca, as well as many other devices & techniques to revise scars. This nurse led clinic is established for patients to get effective treatments for acne scars in cases where there is no Medicare rebate. This provides a cost saving to patients, whilst still having the absolute best access to lasers. Nurse led scar revision ranges from $690 to $1,290, depending on the complexity of revision. For a no obligation assessment with the nurses contact @cliniccutis for appointment times.
When is treatment considered successful?
There are multiple ways to gauge treatment endpoints, none of which are completely accurate, nor practical in real life. Dermatologists & plastic surgeons often use the 70% rule, namely if we can get 70% improvement at the end of treatment/s this is a realistic goal. I am also guilty of quoting this finish line. Nowadays I have another opinion on end points- skip to the end if you want the short of it, read more if you would like to know the logic behind this.
OK, what does 70% improvement really mean is it-
- 70% of your scars can not be seen after treatment. If you have 100 scars, you will only be left with 30 at the end?
- 70% volume reduction of atrophic scars based upon volumetric computation. Namely if you have say a total of 1ml volumetric deficit on your cheek (atrophy), you now have 0.3 ml
- 70% reduction of pigment, either red PIE or brown PIH
- Your scars have gone from being visible at 5 meters to now being visible at 1.5 meters?
- You feel 70% more secure about your scars?
- The impact of scarring is 70% better?
- You spend 70% less time thinking about your scars?
- Only 70% of people can see your scars at conversational distances?
Get the picture? Many ways to quantify 70%, with neither right or wrong answers.
I feel a good end point is to give patients a distance of which they feel or should feel confident at. This is what I call the modified Goodman Baron scale, it is primarily based upon distance. A healthy endpoint is to give patients the realisation & confidence to understand-know & believe that scar revision is successful when other people can not perceive your scarring at conversational distances in normal lighting conditions.


View our Treatment Gallery
What is the best way to monitor my scar revision progress?
Objective photography is the best way to understand your progress. I encourage you to take photos with your phone, then review your progress 4-6 weeks after each revision session. The best way to gauge progress is to ask a friend or a family member to look at the photos & give their feedback. This way you are getting an objective viewpoint.
You might find it helpful to look at one area at a time, for example, examine the cheek one at a time, then the chin, nose, temples, forehead. This way you can make a logical sequential picture in your mind as to your progress.
Subjective assessment is also useful, however it is important to make a decision based upon how others perceive you, namely from the sides & front. Assessing scars at hand held mirror distance ( 25 to 40 cm) in overcast lighting is not how the world sees you. This is probably not the best way to assess your progress.
Why are my scars responding slower than what is expected?
Everything being equal, your progress depends on your genetic make up & your immune’s system’s ability to remodel scars & generate new scarless tissue (collagen, elastin, hyaluronic acid, ground substance, & in some cases fat).
Human biology, much like height, metabolism, IQ etc.. are represented on a bell curve.
Fast responders lie to the right, slow responders lie to the left of this biological curve.
Of course you can implement healthy lifestyle changes to assist your immune system, namely eat healthily, stop or reduce smoking & sun protect. For more of an understanding regarding examples of fast vs slow responders, find the relevant posts on @101.skin

Can I do anything at home to speed up my treatment?
Yes, you can implement a few things as part of your recovery program in between revision sessions.
Dietary & lifestyle changes: Eat a healthy & well balanced diet. Reduce alcohol intake & smoking.
Skin care: Most importantly, above all else, use sunscreen regularly. This protects your skin from UV that may slow down collagen production & prolong skin pigmentation changes including redness, known as post inflammatory erythema (almost predictable with TCA or Phenol Chemical Peels, or ablative lasers) or brown post inflammatory hyperpigmentation. In some cases retinol based products or niacinamide (B3) can aid in collagen production & decrease inflammatory processes respectively. Timing is essential if topicals are used, as your skin’s healing time will depend on the procedure.
Sensible at home treatments: especially pertaining to overseas or interstate patients who can only see me once every few months. In SOME cases the use of sensible dermastamping or DIY derma rollers can be a SAFE way to adjunctively manage SOME forms of acne scars. Needle length for SAFE at home use is in the region of 0.25 to 0.3 mm. IF you are suitable for @home DIY treatments either myself or my staff will direct you at the time of the consultation & or procedure.

How can I arrange a second option?
I am absolutely OK with patients having second opinions as there are many roads to the same destination. If required I can forward your clinical notes to the dermatologist of your choice. My peers include the following dermatologists-
- Dr Robert Sinclair BNE
- Dr Shawn Richard SYD
- Dr Adrian Lim SYD
- Assoc Prof Greg Goodman MEL
- Assoc Prof Philip Bekhor MEL
- This is NOT a comprehensive list of dermatologists, it is just who I know in Australia that can utilize similar methods including laser, peels, surgery, & hydrating treatments to treat & improve acne scars.
One of the most important aspects of scar revision is to establish a therapeutic relationship with the patient. Each doctor has a specific way of practice. To sum up my practice, I am-
- Straight to the point. No fluff with things.
- Respectful of your opinions, however, I will be quick to refer if I can not establish a professional relationship with my patients early in their course of treatments.
- I am also aware that I may not be the best doctor for your personality
- I do not have any expertise to treat BDD (Body Dyspmorphic Patients). For this group of patients, I do believe that a psychologist or a psychiatrist can assist patients more than what my skill levels can deliver. I am NOT interested in placing patients on acne scar revision programs if they are not satisfied with the outcome.
- My motto is ‘Alway treat a problem with a solution that is smaller than the problem itself.’ This means if one has ‘small’ or fine scarring, such as enlarged pores, I will be conservative in my approach, whilst patients with clinically severe scars will be safely treated with surgical, peel & laser modalities.
