- Best ResultsAre very rare
- Treatment Recovery0-1 days
- Procedure Time10-20 minutes
- Skin SpecialistNot performed
- Duration of ResultsMakes melasma worse
- AnaestheticNA
- Back to Work0-1 days
- Cost $-$$
Melasma Microneedlng
Microneedling is an excellent treatment modality for many skin conditions. Melasma is not one of them. In most cases, microneedling worsens this condition. The gold standard for treating melasma is a combination of sun protection, pigment inhibitors & ultra short pulse duration lasers. Sun protection has to be paramount for effective pigment fading. Picosure Pro provides the fastest clearances with the least amount of side effects.
FactsFacts on Melasma Microneedlng
- Microneedling is an effective dermatological treatment for improving skin texture
- It is best utilized to enhance absorption of topicals
- This is achieved with conservative needle lengths of 0.1 mm
- Microneedling is not a great treatment for melasma however can improve skin quality
- Pico lasers offer faster & more effective clearances of pigmentation
- Melasma treatment is multimodality, namely UV protection, topicals, & pico lasers
What is microneedling?
Melasma Microneedlng
As the name suggests, microneedling uses tiny needles to break the surface of the skin. Needles can be delivered via four ways-
- A roller, also known as a dermal roller
- A pen, also known as derma pen, or skin pen
- A stamping device, known as a derma stamper
- A needle that penetrates the skin & delivers energy, also known as RFM or radiofrequency microneedling
What was the original concept of microneedling for melasma?
To increase penetration of topicals, namely mesotherapy. This got lost in translation as beauticians (and even dermatologists) went for deeper needles. This really screwed up the real purpose of needling. There is nothing wrong with the logic of microneedling as it was intended for melasma.
What went wrong was the extension of needling to stimulate collagen production via direct dermal remodelling. This meant deeper needles.
This resulted in a diversion of the initial intention of it’s real purpose. Sticking to very superficial needles that only cause controlled epidermal injury, namely, to breach the stratum corneum (to allow increased absorption of tyrosinase inhibitors) then the logic is plausible.

The problem lies in the fact the most microneedling treatments are too deep. This results in ‘dermal drop out of pigment’. The result? Worsening of melasma pigment.
Why does it make melasma worse?
Many providers use needles that extend into the dermis. This compromises the basement membrane (BM, the layer that separates the top part of the skin, the epidermis from the dermal layer).

Pigment cells live in the epidermis. In melasma there is often a ‘leaky’ BM. Breaking the BM results in more melanocytes to drop out into the dermis, this results in dermal melasma / dermal melanocytosis. This makes melasma worse & harder to treat.
What is the consensus for treating melasma, without the marketing bullsh*t?
Melasma should be approached with science, & not marketing. Here are the tiers of melasma management based upon science. Your dermatologist will guide you through this treatment ladder.
First tier: absolute sun protection. Hats, umbrellas, tinting, plus sunscreen. Use a high factor SPF twice a day, regardless of sun exposure.
Second tier: pigment inhibitors. This includes hydroquinone, arbutin, ascorbic acid, Kojic acid, azelaic acids, & botanicals such as bearberry.
Third tier: plasminogen modulators & vascular modifiers including tranexamic acid, either topically or better still orally.
Fourth tier: lasers including pico lasers, QSL nano or dermal toning. AHA peels.
Fifth tier: lasers including low energy thulium, vascular. Novel peels.


What is the FASTEST way of treating melasma pigmentation?
Pico lasers combined with medical therapy provides the fastest clearance of pigmentation with the least amount of side effects. Effects can be seen as early as one week with the Picosure Pro laser.
Lasers target pigment within the skin, whilst topical creams suppress pigmentation by inhibiting an enzyme in pigment producing cells called melanocytes.

View our Treatment Gallery
Why is melasma different from other causes of pigmentation?
Put simply it is genetic. Technically it’s genetic with a drive from external factors including UV, hormones, heat & iatrogenic causes.
The idea of treating melasma is to decrease the output of melanin (pigment) from melanocytes. Sounds easy, but it is far, far more complicated. There are many factors that dermatologists consider including contribution from blood vessels, basement membrane integrity, hormonal input & sources of radiation (UV to IR spectrum).
What is the concept of lasers for melasma?
Lasers employed for the treatment of melasma do one of five things-
- They reduce pigment transfer from the pigment cell to the skin cells. It is called selective photothermolysis, in other words putting the pigment cell to sleep & not beat the sh*t of out if.
- Increase absorption of topicals that quieten down the pigment cell. An example is low power, low density thulium lasers.
- Repair the leaky basement membrane. High risk, but in theory it can be done.
- Reduce the blood vessels that interact with pigment cells. This is the job of vascular lasers & yellow light lasers.
- Encourage transepidermal & dermal exfoliation of pigment. This was how 1550 Fraxel got approved. Looking back, it was a silly way of treating primary melasma, but it can be used as last line treatment.
For all the patients at Cutis, here is our melasma strategy. All patients are assigned a personal nurse or therapist. Be guided by them-
.
🙄👉De-pigmentation phase: Continue with your prescribed strength of HQ, T.acid, & laser fluence (including intervals), titrate according to skin irritation
.
👍🏻Maintenance phase: Non-HQ suspects (arbutin, ascorbic, kojic, salicylic, lactic, citric acids, botanicals, cysteamine etc..). Lasers spaced out to 3-4+ weeks. Cease orals. This phase will vary depending on your goals, expectations & melasma. Your timing to go back to the depigmentation phase will be determined by you & your treating clinician
.
👉For some patients, you will be transitioning to a new laser platform; the Hollywood Spectra by Lutonic in the upcoming week/s
.
🔫What is the Hollywood (corny name) Spectra? Replacement for the Spectra. It’s a super powered short pulse duration Q switch laser. Improvements over the older gen include- ability to fractionate the beam, flat top beam profile,& crazy power (though for melasma that is irrelevant, consistency is more important). Stay tuned for B+A from our laser nurses at Cutis Dermatology💯
.
😎Dr Davin Lim
Dermatologist
Cutis Dermatology
Brisbane🇦🇺
.
#pigmentationcure #melasma #skinlightening #skinbrightening #melasmacure #melasmatreatments #pigmentationcure #melasmapeels #melasmalaser #drdavinlim #dermatologistbrisbane #spectralaser #hollywoodspectra #lutronicspectra
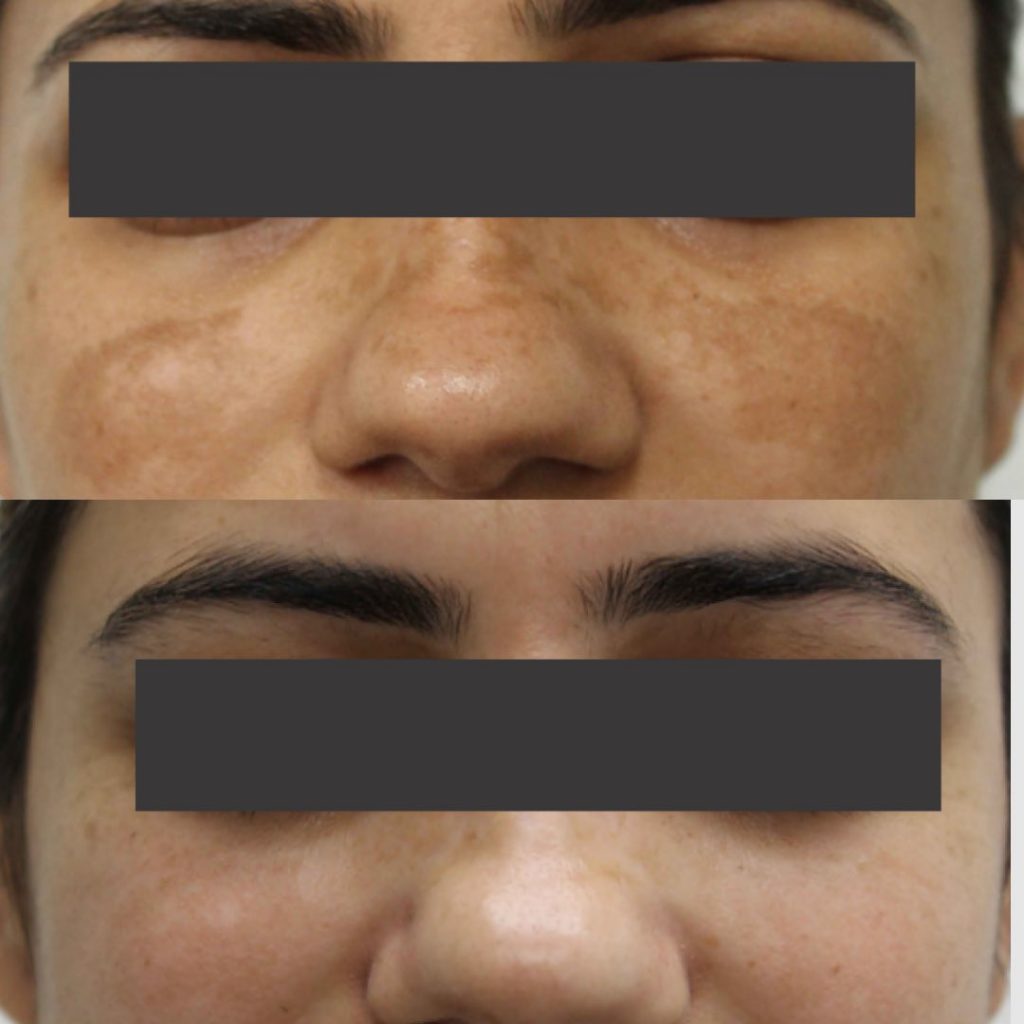
You can still achieve great results with older technology. This post demonstrates the efficacy of dermal toning, using nanosecond Q switching, 1064 wavelength
.
👍🏻Concept: subcellular selective photothermolysis; namely reduce melanocyte activity without blowing sh*t up. 💥Over cook it & the melanocyte will react by increasing pigment production. 🥊This is the basis behind melasma treatments. Long wavelength 1064, penetrates into the deeper dermal layers with resulting neocollagenesis (collagen production). This translates to less pigment, more collagen, reduction of fine lines, wrinkles, textural changes & enlarged pores
.
📸This B+A shows skin aging in reverse. The patient’s age in 50, & she has better skin quality now cf when she was 44
.
🎬Action: For this treatment, book a consultation with our nurses at Cutis Dermatology, yes we are in BrisVegas not Nigeria
.
😎Davin Lim
Dermatologist
Brisbane 🇦🇺
.
#dermaltoning #skinrejuvenation #skincaretips #melasmatips #dermatologistbrisbane #dermatology #drdavinlim #skinbrightening #skinlightening #skinquality
This B&A is from nano QSL, not a pico. It illustrates that with correct settings & passes, the results from older tech can still be very good. Overpassing in this region is relatively safe as melasma is usually limited to areas BEYOND the orbital rim. We used the older Spectra Lutronic laser for this job🔫
.
😎Davin Lim
Dermatologist
Brisbane🇦🇺
.
#dermaltoning #spectralaser #spectrahollywood #revlite #darkcircles #melasma #pigmentation #dermatologist #drdavinlim #davinlim #brisbanedermatologist #skindoctor #cutisdermatology
Melasma management by Lara @cutis.dermatology
.
👍🏻Medical mx: Tyrosinase inhibitors & t.acid
.
🔫Laser: Nano QSL @lutronicaustralia Spectra
.
👌🏻Next rotation: L-ascorbic topically, QSL maintenance
.
👍🏻Next round of depigmentation: in 3 months time when UV index is lower
.
😎Davin Lim
Dermatologist
Brisbane🇦🇺
#dermatology #dermatologist #melasma #pigment #skinbrightening #skinlightening
#skincare #glowingskin
Picoway laser. 2 sessions for melasma
.
👊🏽Melasma management: is medical. Namely tyrosinse inhibitors & plasminogen /VEGF modifiers coupled with reducing exposure to UVB, UVA, visible & IR radiation
.
🔫Lasers are useful adjunctively: this result was by Jean @cliniccutis using Candela’s Picoway with the 6 mm spot at both full beam & fractional settings, 1064 nm
.
🔍Note: improvement in skin texture & quality as well as reduction in pigmentation
.
😎Davin Lim
Dermatologist
Brisbane🇦🇺
.
#melasma #melasmatips #pigmentation #PIH #melasmacure #melasmaskincare
#treatingmelasma #laserskintoning #skinlightening #skinbrightening #drdavinlim #dermatologistbrisbane
Why do I like Picosure Pro for melasma?
Picosure Pro is the best laser for melasma pigment (better than Picoway). It provides super fast clearance of melasma within 5 to 10 days in one single treatment, however a series of 4-5 sessions will give better results.
Pico lasers can deliver laser light that breaks up unwanted pigment with super high energies but very little heating- that is the key in treating melasma pigment.

Pico lasers are most useful for treating all forms of pigment, including melasma. Lasers should always be combined with medical therapy for optimal results. Using appropriate technology we can clear most, but not all cases of melasma. Our hit rate ranges from 80 to 85%.

What about chemical peels?
Maybe you don’t have access to lasers. Peels can help. The thing to remember is that peels must be gentle. My preference is glycolic or lactic acid, low concentration at 15 to 25%. Peels work by exfoliation of pigment, they do not suppress melanin production, hence they are not my preferred method.

What is Dermamelan & Cosmelan?

There are novel peels. I use these peels if-
- Patients cannot have lasers, namely geographical constraints.
- Melasma is primarily epidermal, or mixed.
- The patient understands photoprotection
- Ideally patients are on vascular moduators
What is tranexamic acid?
Tranexamic acid is a plasminogen & vascular modulator. Most dermatologists use this tablet to reduce vascular input to your pigment cells. This is a prescription tablet. Your specialist will take an appropriate medical history to ensure you do not have any contraindications. Tablets are far more effective than creams.

What happens if your melasma got worse with microneedling?
I may be able to help you, depending on how bad things are. If your melasma is dermal (grey, dusky), it is much harder. I would rather treat epidermal flare ups from IPL compared to deep microneedling exacerbated dermal melasma.

Can I improve all types of melasma?
I can improve 80-90% of cases. Despite optimal sun protection, pigment inhibitors, tablets, lasers & peels, 10-20% of cases of melasma are resistant.
We are in an infinitely better position to treat melasma now than ever before. Perhaps in the next decade more research will reveal better solutions for resistant melama.

Why is sun protection so important?
50 percent of pigmentation can fade with proper sun protection. This means hats, umbrellas, tinting as well as sunscreens. Use a high factor SPF 50+, minimum of four mls a day. You should use a 50ml tube within 2 to 3 weeks.
If you don’t take sun protection seriously you are wasting your time, effort and money trying to fix your pigmentation.
What other factors flare up melasma?
Hormones & heat. Melamsa can worsen with pregnancy & IVF. Additionally, heat generates IR or infrared radiation. This can worsen pigmentation. Sources of IR include cooking and saunas. You don’t really need to worry about computer screens as a primary source of heat & radiation until you get your photoprotection down pat.
Who to see for melasma treatment?
Book an appointment with my nursing team at Clinic Cutis. They have been taught how to assess & treat the majority of melasma cases. I can provide input for more challenging cases or if the diagnosis is in doubt.
My team will treat your pigment, without the hard sell. We view melasma as a medical condition, so you won’t be hammered with expensive packages.
Sydney patients can book here.
What if you really want to try microneedling?
OK, let’s say you wanna give it a go, what now? If you are insistent on microneedling as the treatment of choice based upon your research, you can ‘give it a go.’ Here are some hints to do it safely.
- Use a max of 0.1 mm, that’s right 1/10 of a millimetre. This is the approximate thickness of your epidermis.
- Use a stamper over a roller or a pen. With a stamper you can’t go deeper than the needle. With a pen you have the temptation of rotating that dial to go deeper, and deeper, then deeper still.
- Make sure your sun protection is absolute. This means SPF like twice a day minimum, hats, umbrellas, tints etc…
- Make sure your pigment cells are asleep. See a dermatologist for prescription creams & pigment inhibitors.
- If you must, stamp once every 7 to 14 days. Stamping is designed to increase penetration of topicals. If you break the basement membrane of your skin, it is counterproductive *in the context of melasma management
- Take photos, do a comparison. This is the only way you are going to get an objective assessment of your pigmentation.

Rebound melasma from microneedling is darn hard to treat. If you must micro needle, keep the depth to 0.1 mm or 100 microns.
What is a simple skin care routine for pigmentation?
A simple, cost effective way to improve pigment is as follows-
- Sunscreen twice a day. 50+ in the AM with an aerosol application in the PM
- Antioxidants in the AM (Before sunscreen). Look for vitamin C, E, ferulic acid.
- Azelaic acid in the evening. You can add a retinoid such as tretinoin 1-2 nights a week as tolerated.
Whilst DIY treatments may not clear all of your pigment, this routine is far safer than microneedling (in the context of melasma treatments).
Davin’s Viewpoint on microneedling for melasma
Wow, what a spike in cases over the past two to three years. This follows the upward trend of using microneedling for everything, including melasma, skin rejuvenation, wrinkles, acne scars, hair loss, dark circles, & haemorrhoids. Maybe not the last condition, but you get the drift. I am not against microneedling- I use it daily, however not for melasma. If I had a choice between microneedling versus a simple pigment inhibitor such as azelaic acid, my preference is azelaic acid as this won’t worsen melasma. Rebound melasma from microneedling is one of the harder types of melasma my team & I have to deal with. IPL flare ups, though spectacular, is relatively easy to treat as most cases are epidermal (superficial). Deep melasma is much harder to treat, with success rates below 30% (in comparison to normal melasma, whereby our success rate ranges from 80-85%).


If we catch micro needling stuff ups early enough, we can make a difference. If not, it is difficult to improve dermal drop out. It is not that I am against microneedling, as I use this daily to treat scars, mainly to increase the absorption of CS topically. Providers just need to apply the correct indication for a treatment. For more on melasma, book an appointment with my clinical staff at Cutis Dermatology.
For Sydney patients, book an appointment with Louise at Dr Van Park’s practice in the Eastern Suburbs. I will be consulting on select pigment cases in early 2024.

