Filler Side Effects, At A Glance
- Best ResultsDepends
- Treatment RecoveryVariable
- Procedure TimeDepend on complication
- Skin SpecialistDermatologist
- Duration of ResultsNA
- AnaestheticNil
- Back to WorkDepend on complication
- CostVariable
Hydration treatments, side effects
Side effects following hydrating treatments are increasing in number. Part of the reason is the enormous increase in the number of procedures over the past few years. In Australia, cosmetic GPs, specialists, dentists or nurses can inject hydrating treatments. It is important to understand the risks of hydrating treatments, as some side effects are permanent.
FactsFacts on Skin Hydrator Side Effects
- Filler side effects are rare in comparison to the numbers
- Common side effects include bruising, & swelling
- Uncommon side effects include persistent lumps
- Rare side effects include infection & artery injection
- Extremely rare side effects include blindness
What are the most common side effects of hydrating treatments?
Bruising, asymmetry, lumps & bumps. The majority of side effects are mild, transient, & in most cases will resolve with time. Bruising is more common with needles over cannula. Bruising is more common in multiple injection sites, locations such as the lips or around the mouth. Other factors include medications, supplements (fish oil, vitamin E, St John’s Wort) as well as injector technique.
Filler asymmetry is most common on the lips & nose (midline structures). A small amount of asymmetry is normal & acceptable for cheek hydrating treatments, temple, jowls, & hydrating treatments around the eyes. The majority of cases do not require correction. If required, your injectable provider can discuss ways to correct asymmetry. In most cases it involves placing a tiny amount of hydration treatment on the other side. In other cases, it may involve dissolving an extremely small volume on the overcorrected side (harder job).
How long will bruising or skin discolouration last?
Bruising may last up to two weeks. This is self-limiting, however resolution can be sped up considerably with V-BEAM or vascular laser. Lasers can halve the time to clearance. Arnica cream can marginally improve bruises.
Delayed ‘new vessel formation’ or neovascularization is very rare, as are persistent iron staining of the skin due to bleeding. The former is easy to treat, the latter is more complicated. Haematoma formation or blood clots under your skin can rarely happen (less than 1%). The chances of clots can be reduced with avoidance of certain medications including vitamin E, & fish oil, careful injection technique (cannula vs needles), & most importantly compression after the event. All early haematomas should be evaluated & evacuated to prevent fibrosis or encapsulation (hardening). The latter should be differentiated from nodules due to hydration treatment or delayed onset nodules. If required, your injector – doctor can arrange an ultrasound.
Persistent bruising & discolouration can be treated with nano or pico lasers.
What does arterial or vascular occlusion mean?
This is when hydration treatment is inadvertently injected into an artery. The hydration treatment is then lodged in smaller end arteries & capillaries. Depending on the location of the injection, the overlying skin’s oxygen supply is compromised leading to necrosis or skin death.

This can be reversed if skin hydrating treatments are used, & if intervention is timely. Vascular compromise is most commonly seen following hydrating treatments in the nose & forehead area, however, have been reported around the lips, cheeks, chin & other areas of the face.
How do I know if hydration treatment has been injected into a vessel?
Your injector will probably know before you do. Arterial hydration treatment injections, contrary to literature review, are not painful during the event itself. Pain is often delayed for a few hours. Over the next few hours, the overlying skin turns a mottled pink to red colour. The area involved can be focal, or it can be extensive if a major artery is injected. The colour changes following intravascular injection goes from white to pink, then red, then purple, then dusky grey then black. Timeline ranges from 4 hours to 36/48 hours. Sterile pustules may form prior to skin breakdown. The majority of cases are painful.
In some cases, your injector will realise that an arterial vessel has been injected. They may see a ‘flash’ as hydration treatment makes its way to the end capillaries, additional the skin may turn pale due to occlusion. Capillary or blood refill is compromised. In other cases, there are no clues. Be guided by your injector, as we all have different protocols for follow ups.
If you think you may have an occlusion, contact YOUR injector.

View our Treatment Gallery
What should you do if you suspect you have an arterial injection incident?
Be guided by your injector. We all have different protocols regarding acute emergencies. The consensus is that patients are seen immediately, & hydration treatment dissolving agents be administered immediately. This applies to hyaluronic acid (HA) based hydrating treatments.

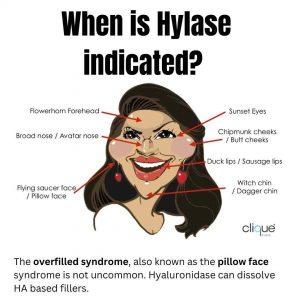
HA hydrating treatments can be reversed by an enzyme called hyaluronidase or Hyalase. For reversal of blocked vessels, most injectors will repeat this process 1-2 hours after the initial injection as the half-life of Hyalase is short. In some cases, this is repeated several times until we know that your tissue has the oxygen supply back. In other cases various tablets are prescribed adjunctively to help with blood flow and O2 levels, including aspirin, & nifedipine. In extreme cases hyperbaric oxygen can be an adjunctive treatment.
In summary- if you think you are suffering from a vascular event, contact your injector. If they are not contactable, visit your emergency department as soon as possible.
Can you go blind with skin hydrating treatment injections?
Blindness has been reported with both hydrating treatments & fat transfer procedures. There have been several cases reported in Australia. Extensive knowledge of anatomy, the use of cannulas & injection techniques can reduce but not prevent hydration treatment associated blindness.

The incidence of blindness is higher in Asian countries due possibly to training & regulations, but also the fact that higher risk areas are being treated. High(er) risk areas include the glabella or frown area, nose & the forehead. There have been cases of blindness following lip injections, however in the scheme of things, this is extremely rare. The risk benefit ratio will be discussed with your injector prior to the procedure.
Can blindness from hydrating treatments be reversed?
At the time of writing there are only two documented cases of reversal of blindness following skin hydrating treatment injections (G. Goodman in Australia, & C.Chestnut in the United States). There are many more cases of irreversible blindness compared to transient blindness or reversible vision loss in the literature.



What causes nodules or lumps following hydrating treatments injections?
Complex question, a simplified answer is:
Early nodules or lumps: most commonly due to product & or injector. Normal to ‘feel’ lumps, especially for the first 2 weeks. Lumps can be due to product (either too much product or wrong product), or haematoma (bruise) from the procedure itself. Majority will resolve without any intervention. If too much product has been placed, your injector may elect to dissolve this with Hyalase (if HA hydration treatment) or inject with saline solution to hyper dilute the area. Subcision is very rarely used. Be guided by your injector.

Delayed nodules or lumps: Much more complex. Most commonly seen with Vycross hydrating treatments such as Juvederm. These hydrating treatments made by Allergan are very popular, hence maybe over-represented. The majority of these delayed nodules are transient & do not require dissolving. They can occur with viral infections & immunizations including the latest Covid Modena vaccine. Your injector will determine the cause of theses nodules & will dictate action based upon history & clinical findings.
Other hydrating treatments include collagen stimulating hydrating treatments such as Polymer Injectable, Polymer, PCA Ellanse, Bellafill, PMMA or Artefill. Silicone hydrating treatments are still used by many countries, including Korea & China. Filler reactions following this group of hydrating treatments can be complex to manage. Treatments range from saline injections, incision, USS guided fibre laser ablation, excision, 5FU & dilute steroid injections.
How do specialists manage lumps?
Diagnosis before treatment. A good history is essential as it gives clues as to the diagnosis. It is most important to give me as much information as possible in order to help you. I do require important information including the type of hydration treatment, volume & location injected. I may have to work with a team of plastic surgeons, imaging specialists & infectious disease physicians in some, but not all cases.
Imaging may be required in some cases, either USS (Ultrasound) or MRI scans to ascertain the exact location & amount of skin hydrating treatment .

Biopsy may be required in some cases. Histology, culture for bacteria, typical & atypical infections are often submitted during the time of biopsy, PCR is often requested at the same time.
I do require a referral from your injector or cosmetic doctor with all the information including the sites of injection. This includes a FULL HISTORY – even if injections were performed two decades ago.
How rare is infection following hydrating treatments & how to treat?
Fortunately, infections following hydrating treatments are rare, apart from cold sores. This common infection is due to reactivation of cold sores, or HSV (herpes simplex virus), often secondary to lip hydration treatment injections. Your injector will cover you with antivirals prior to lip fillers.
Bacterial infections are much rarer & include cellulitis or abscess. These are ‘acute’ or ‘subacute’ events that usually occur within 24 hrs to one week.

Biofilm infections are rare, and usually present weeks to months/years after injections. These can be difficult to diagnose & treat. The majority of ‘biofilm’ reactions I see are usually due to non-inflamed delayed nodules (most commonly seen with Biostimulator Vycross hydrating treatments). Biostimulator nodules may be over-represented as this is the most commonly injected brand by Allergan.

Do all lumps require dissolving or intervention?
No. Depending on the clinical scenario, not all nodules (lumps) require intervention. A good guide is that if an asymptomatic lump can be felt but not seen, it usually does not require treatment as most will resolve with time. Exceptions are if nodules are symptomatic, & or if the patient is immune compromised.
In rare cases your specialist may elect to inject around the lump-nodule to disguise it. An in-depth consult discussing all the risks is required if this avenue is to be considered.
Why is my undereye area / tear trough area blue?
This is called the Tyndall effect & is due to the absorption of red light due to hyaluronic acid hydrating treatments. Tyndall can occur due to the following reasons-
- hydrating treatment selection was incorrect
- hydrating treatment placement was incorrect
- Concentration of HA too high
- hydrating treatment migration
- Combination of points 1 to 4
- Lighter skin complexion will show Tyndall cf. darker skin types
Tyndall is a very common side effect of hydrating treatments placed in the tear trough. Not all forms of Tyndall require reversal, especially if it is mild & or able to be covered up with makeup. Treatment is with hyaluronidase by your injector.

Who should manage your skin hydrating treatment side effects?
Ethically, your injector has the responsibility of managing your skin hydrating treatment reaction. If one is legally allowed to perform a procedure, either the injector & or their supervisor will know how to manage common side effects such as bruising, swelling, early & delayed lumps, as well as rare side effects such as arterial compromise or compression, & infections.
Hyaluronidase or hydration treatment dissolving should ideally be done by your injector as he or she will have a ‘road map’ as to the brand of the hydration treatment, volume amount, layering, & exact location. As a dermatologist I am more than happy to provide input for unusual – complex cases. You will require a referral from a GP (Medicare rules, not mine).
Davin’s take on skin hydrating treatment safety
I have been fortunate enough to have completed my dermatology specialist qualifications just when hydrating treatments were still at their initial stages of mainstream popularity. I remember as part of my board exams, dermatologists had to know how to ‘patch test’ with bovine collagen!
Filler technology & selection has seen double digit growth year after for the past two decades. Along with the ‘classes; of hydrating treatments, we have many brands in Australia, with new releases every few months. Those in the industry know that obtaining TGA approval (or FDA, CE for that matter), does not reflect the actual safety profile of hydrating treatments. Practicing as a procedural dermatologist, I get to see the pointy end of side effects. Everything ranging from biofilm, delayed nodules, inflamed nodules, infection, hydration treatment migration, & many others.
I do believe the industry as a whole requires better education, especially when it comes to managing the side effects of procedures. If one is allowed to perform the procedure, one should manage the common side effects. Hopefully with continued meetings & education, specialists, cosmetic GPs & nurse injectors will continue to learn not only new techniques, but to better understand the side effects of the injectables we deliver to our patients several times a day.

I am more than happy to supervise or manage difficult & unusual hydration treatment cases referred by my injector colleagues. I do believe that the injector has primary responsibility for any cases (this is how I practice my injectables), however if your provider requires some assistance for complex cases, I will intervene. A referral from your GP or specialist is required under Medicare best practice as I am a specialist.

